Autism & Acetaminophen: Five Myths vs. FiveTruths
From a Mother and Disability Specialist
Disability Specialist

While this has been a topic of discussion for years, it has recently resurfaced with a once respected governmental agency backing its rhetoric. The discussion that surrounds the "cause & cure for Autism" has always given me an ache in a strange place. The metaphoric ache isn't because I wouldn't want to know the "cause & cure for Autism". I am the mother of a son with Autism and I have advocated for people with Autism for over 10 years. This metaphoric ache is because the people that speak with the most convincing tones & largest platforms often haven't utilized true scientific evidence for the information they spread. With the world of social media shifting the way information is relayed and received, it is important that we carefully review information before spreading it to others in our networks.
Lately you’ve probably seen headlines (and lawsuits) claiming that taking acetaminophen (brand name Tylenol®) during pregnancy “causes” Autism. Families deserve clarity, not clickbait. Here’s a plain-language guide to what the science actually shows—and what major medical organizations currently recommend.
- Myth #1: “Taking acetaminophen during pregnancy causes Autism.”
Truth: The cause has not been proven.
Some earlier studies (including those measuring acetaminophen metabolites in cord blood) found statistical associations with autism or ADHD. Metabolite may refer to the product that remains after a medicine is broken down (metabolized) by the body. However associations can arise from other factors, such as the illness prompting the medication (fever or infection), genetics, or family environment. There is research available
from 2019 that states when researchers used a stronger design—sibling controls in a nationwide cohort of 2.48 million births—the association disappeared.
- Myth #2: “There’s a medical consensus that acetaminophen is unsafe in pregnancy."
As of today, there is no clear evidence that proves a direct relationship between the use of acetaminophen in any trimester and fetal developmental issues. The guidance on use has not changed. As with any medication, discuss the use of medication with your clinician.
- Myth #3: “Headlines and lawsuits prove the link between acetaminophen & Autism.”
Truth: Legal claims and media cycles aren’t proof that this is true.
Unfortunately, there are legal claims that hit out court system daily. In fact, in 2022, a court case
was filed to discuss the linkage between acetaminophen and ADHD (Attention Deficit Hyperactivity Disorder. In 2024, the court excluded general-causation experts and issued orders unfavorable to plaintiffs because their methods didn’t meet evidentiary standards. Court outcomes aside, science is decided in studies, not in courtrooms.
- Myth #4: “Any use is risky; it is better to avoid acetaminophen completely.”
Truth: Context matters, and an untreated fever can itself pose risks.
Studies that report higher risk often involve frequent or prolonged use and can’t fully separate the effects of the underlying condition (e.g., fever, infection, migraine) from the medicine. The large 2024 sibling-analysis
found no dose-response pattern once family factors were controlled. Meanwhile, maternal support groups & medical professionals emphasize treating fever/pain appropriately during pregnancy.
- Myth #5: “Autism has a single preventable cause.”
Truth: Autism is multifactorial and primarily neurodevelopmental with strong genetic contributions. Recognized risk factors include having a sibling with autism and certain genetic conditions. Prior to Robert F. Kennedy Jr. being appointed as the secretary of health and human services, acetaminophen was not listed by the CDC among established risk factors.
So…what should families do right now?
- Talk to your clinician before starting or changing any medicine in pregnancy.
- If acetaminophen is advised, follow your clinician's guidelines as they have full details on your overall health.
- Don’t ignore a fever during pregnancy. Get guidance on when to treat and when to be seen.
- Keep perspective because one study rarely settles complex questions. Prioritize high-quality design studies (e.g., sibling/within-family comparisons) over headlines.
- Remain connected to a support group that shares your values. With all of the clickbait news coming out, you will want to connect with others that respect your decisions for your family.
Note: This post is educational and not medical advice for any individual. If you’re pregnant or planning pregnancy, please speak with your own healthcare provider about your situation.
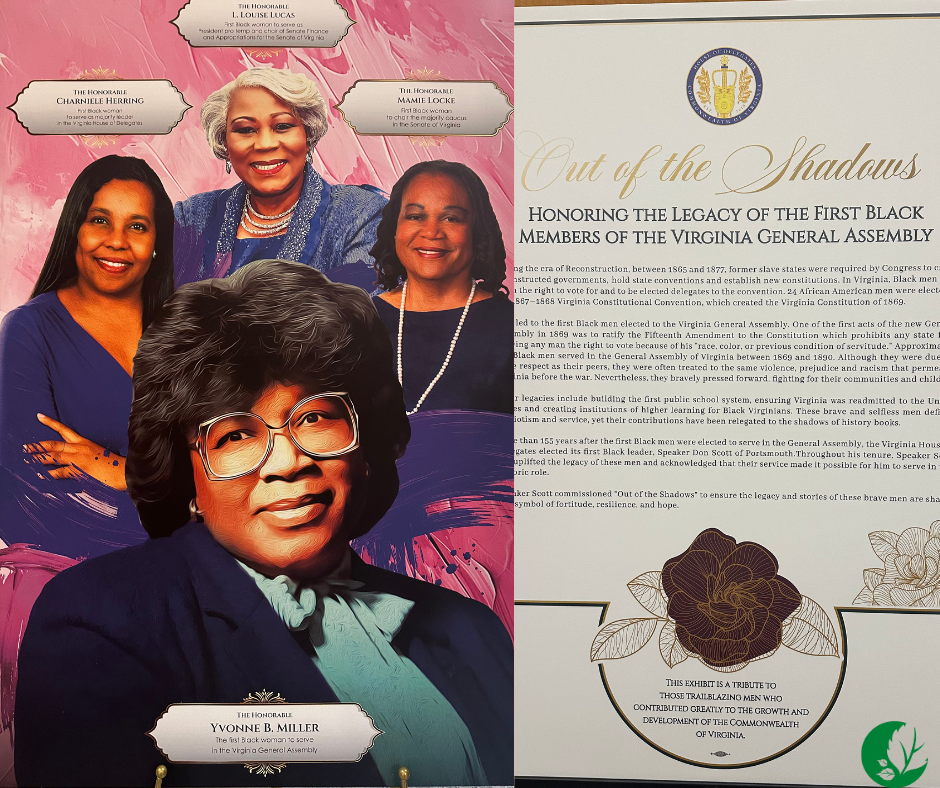
A week has passed since I attended the “Out of The Shadows” Annual Breakfast Recognizing the Contributions of African Americans to the General Assembly. This year’s event recognized the contributions of The Honorable L.Louise Lucas, The Honorable Charniele Herring,The Honorable Yvonne B. Miller, and The Honorable Mamie Locke. The Honorable L.Louise Lucas served as the first black woman to serve as President pro temp and chair of Senate Finance and Appropriations for the Senate of Virginia. The Honorable Charniele Herring served as the first black woman to serve as majority leader in the Virginia House of Delegates. The Honorable Yvonne B. Miller served as the first black woman to serve in the Virginia General Assembly. The Honorable Mamie Locke served as the first black woman to chair the majority caucus in the Senate of Virginia. It was truly an honor to attend this private event and recognize the contributions of these women. Each person on the program spoke highly about the contributions they have made to Virginia. I felt so inspired about my own journey into advocacy and policy initiatives by the end of the event. I had the pleasure of spending the day meeting other change makers in Virginia as well. I spent the most time speaking and connecting with Delegate Jackie Hope Glass. If you haven’t made an appointment to visit her, you should do it right away. She welcomes guests with such a large smile and I was lucky to also be greeted with a hug. Her office has her own curated pieces of art. I was stoked to see her vinyl record collection as well. Delegate Hope Glass inquired about my advocacy efforts and she listened to my responses with such intention. I had the chance to learn more about her naval career and also the committees that she currently serves on within the General Assembly.

The Day I Realized Parenting Is Political I used to think politics lived somewhere far away from my kitchen table. Politics was something that happened in government buildings, on debate stages, or in news headlines scrolling across my phone while I folded laundry. Politics felt optional and very separate from my daily life as a parent. Then one day changed everything. It wasn’t dramatic in the way movies portray turning points. No protest marches. No viral moment. Just me, heading to the pharmacy to pick up my son’s prescription after a long, exhausting day. This wasn’t his first time receiving this prescription, but we changed insurance carriers. Earlier that evening, I had waited on hold with his pediatrician, which was a common reoccurrence in order to request a refill. I had answered their monthly questions & filled out forms that asked me to summarize my child’s updates. The pharmacist welcomed me to the counter and asked for my son’s demographic information. She returned to the counter and recited the total “$476.85”. I’m sure she was using a normal tone of voice, but hearing that number sent a shockwave through my body and I felt like she was whispering. I asked her to repeat herself and when the information didn’t change, I froze in shock. Eventually, I asked her why the price changed so much and she informed me that due to my new deductible not being met, I would pay this total. I made a split decision and purchased it, but felt sick on the ride home. Making this purchase was not included in my budget, but what could I do? I returned home and my children were sound asleep. I cried for a moment. This was so unfair. The insurance carrier was the same, but the type of insurance policy we had was different. How could such a drastic change occur with the stroke of a pen? As I watched my son sleep, questions hit me like a wave: Every challenge I faced that day had been shaped by a policy decision. Why is it that parents aren’t included in these policy decisions? Were parents involved and why wasn’t I asked? Were the policy makers parents as well? That’s when it clicked. Parenting IS political. Not because I suddenly wanted to argue about parties or elections but because systems were shaping my family’s life in ways I could no longer ignore. I saw it in access to healthcare. I saw it in special education services. I saw it in childcare costs. I saw it in waitlists for therapies. I saw it in transportation barriers, food programs, disability supports, and mental health resources. None of those things are accidents. They are outcomes of legislation, funding priorities, and leadership choices. As parents, we make hundreds of decisions every day: what our kids eat, how they learn, how we discipline, how we show love. However, layered underneath those personal choices are public ones. Decisions are made by people we may never meet, determining what resources exist for our families and who gets left behind. That night, I stopped thinking of advocacy as something “extra.” It became part of my job description as a parent. I realized that staying quiet didn’t protect my family. Being overwhelmed didn’t excuse disengagement, and hoping someone else would fix broken systems was not a strategy. I didn’t suddenly become an expert in policy. I didn’t start attending every meeting or reading every bill. What changed was my awareness and my willingness to speak. I started asking questions. Why are families forced to prove hardship over and over just to receive basic support? Why do caregivers burn out while navigating fragmented systems? Why are children’s needs debated as budget line items instead of human realities? And perhaps most importantly: Who is at the table when these decisions are made and why aren’t more parents there? Parenting has taught me that advocacy doesn’t always look loud or polished. Sometimes it looks like sending one email after bedtime. Sometimes it looks like testifying while your voice shakes. Sometimes it looks like sharing your story so another parent feels less alone. Politics isn’t just campaigns and headlines. It’s whether your child gets early intervention. It’s whether your family can afford prescriptions. It’s whether schools have the staffing they need. It’s whether caregivers receive respite. It’s whether disability services are accessible, dignified, and person-centered. Once you see it, you can’t unsee it. And once you realize that parenting is political, you begin to understand that loving your child also means fighting for systems that honor them. I don’t advocate because I enjoy it. I advocate because my family deserves a world that works. I advocate because no family should have to navigate complex systems alone. I advocate because policies written in quiet rooms ripple loudly through our homes. That night beside my child’s bed didn’t make me partisan. It made me intentional. It reminded me that parenting isn’t just about raising children, but it’s about shaping the world they grow up in. And that responsibility belongs to all of us. What is Politics & Parenting? I have visited the Virginia General Assembly building many times. In fact, I have visited government buildings in various states over the years as well. However, witnessing the annual recognition of African American legislators in Virginia lit a spark in me. I returned from Richmond,VA with so much excitement about the bills I have been advocating for passing their respective chambers earlier in the day and for once, I felt hopeful for change. However, as the night went on, I realized that the same families that I am advocating for often don’t know what to do and how to get involved. On the other hand, I thought about how politicians that are also parents use their lived experience to drive policy. Parenting and Politics aims to help families understand how everyday decisions at home connect to policies made in government. It’s about translating complex civic issues into the real-life impact of healthcare, education, disability services, childcare, and community support through the lens of parents and caregivers. By centering our lived experience, Parenting & Politics empowers families to learn, speak up, and advocate for systems that truly support their children and communities.

When people hear “race coordinator,” they often picture clipboards and cones. I picture faces—parents pushing jogging strollers, adults with Autism running with their loved ones, volunteers in bright shirts cheering like they’re at the Olympics. Serving as the 2025 race coordinator for two of our local Autism Society of Tidewater Virginia (ASTV) 5K races (the Annual Superheroes vs Villains 5K-held in April and the Annual Surfers Healing 5K-held in August) has been one of the most meaningful leadership roles I’ve held, because it blends logistics with love, and planning with purpose. Designing a race where everyone belongs From day one, my goal was simple: continue to build upon an event that has been around for over 15 years. I wanted to curate a 5K that works for every body and every nervous system. That meant designing with inclusion at the core, not as an afterthought. • “Quiet Start” & rolling start window. We offered a low-stimulus start option—fewer announcements, softer music, and a wider time window—so runners and walkers could ease into the course without a surge of sound or crowding. We welcomed inclusive run groups from Ainsley’s Angels of America & Team Hoyt Virginia Beach . Both groups are based in Virginia Beach. • Sensory supports. We provided sensory-friendly items to families such as noise-reducing headphones, sunglasses, and fidgets. • Course accessibility . We audited the route for wheelchair and stroller access, created clear color-coded signage, and ensured no one had to guess where to go. Turning a field into a finish line (the operations side) A great race experience is built on invisible systems. I was tasked with coordinating permits, insurance, first responder coverage, and medical support. We also ran a simple “command center” under the ASTV welcome tent for operations, course, and medical. That structure let us solve problems quickly—like re-organizing our vendor setup area because group arrived too early without instructions—without anyone noticing a hiccup. Partnerships, sponsorships, and the heart of fundraising The 5K is more than a morning run; it’s a fundraiser that powers family supports, training, and referral services. I created a tiered sponsorship package with community-friendly options (in-kind snacks, water, and printing) alongside headline opportunities. To make our sponsors feel like partners, we: • Offered activation spaces at the expo so organizations could share resources families actually need. • Built a team fundraising playbook with customizable emails, social posts, and talking points to make peer-to-peer outreach less intimidating. • Recognized supporters on course signage, and bibs. Volunteer orchestration: the real engine Race day doesn’t happen without volunteers. We staffed packet pickup, water tables, finish chute, medal distribution, and clean-up with a mix of high-school students, civic groups, and returning families. I created role-specific descriptions, staggered shift times, and then centralized check-in so no one felt lost. The result: faster set-up, calmer runners, and volunteers who finished their shifts feeling useful and appreciated. Safety, dignity, and data We measured what mattered: average wait times at registration, water usage, and medical calls. I am waiting to receive runner feedback about noise, signage, and crowding. Post-race, we reviewed the numbers and will measure that alongside qualitative comments to decide what to keep, fix, or retire. Stories that stay with me There were two teens who ran their first 5K; the mom who cried happy tears because her son crossed the finish line alone; the mom who beamed with pride as her son independently sang the national anthem before the race; the dance instructor that thoroughly enjoyed warming us up with an inclusive dance session; the volunteer who came “for the service hours” and left asking how to get more involved with the Autism Society. Those moments are the real finish line. What I learned (and what I’ll keep doing) 1. Design for sensory comfort first . When we get that right, everything else—safety, speed, smiles—gets better. 2. Over-communicate in multiple formats . A map + a visual schedule + clear signage beats any single announcement. 3. Train like it matters—because it does. Volunteers are ambassadors; investing in their confidence transforms the day. 4. Make sponsors part of the mission, not just the banner . Activation and storytelling build long-term partners. 5. Debrief with data and compassion. Metrics help; listening to families helps more. Gratitude, always I’m endlessly grateful to our runners, walkers, families, volunteers, sponsors, first responders, and the Autism Society of Tidewater Virginia team who trust me to steward these events. Being race coordinator has shown me how powerful a community can be when inclusion is the plan—not the contingency. If you’re reading this and wondering how to get involved next year: join us. Lace up, volunteer, or sponsor a team. Whether you move fast or prefer a quiet start, there’s a place for you on our course—and in this community we’re building, one finish line at a time.

Transitioning to college is an exciting step, but it can also feel overwhelming—especially for students with disabilities. Navigating this new environment requires understanding your rights and becoming a strong self-advocate. Knowing your rights will empower you to thrive both academically and personally. Here’s a guide to help you get started. Know Your Rights Under the Law As a college student with a disability, you are protected by laws that ensure equal access to education. Here are the key federal protections to be aware of: 1. Americans with Disabilities Act (ADA) • Prohibits discrimination based on disability in public and private colleges. • Requires institutions to provide reasonable accommodations for students with disabilities. 2. Section 504 of the Rehabilitation Act • Ensures that any program or activity receiving federal funding provides accommodations to qualified students with disabilities. 3. Fair Housing Act (FHA) • Protects your right to accessible and equitable housing on campus. Understanding these laws ensures that you know what accommodations and support you’re entitled to and can confidently advocate for them. A few steps to advocate for yourself are listed: 1. Register with Disability Services • Contact the disability services office at your college as early as possible. • Provide documentation of your disability (e.g., medical records, psychological evaluations, IEP/504 plans). 2. Know Your Accommodation Needs • Reflect on the accommodations you’ve used in high school, such as extended test time or note-taking assistance. • Determine whether additional accommodations might help in college (e.g., assistive technology, housing modifications). 3. Communicate Clearly and Professionally • Schedule a meeting with your disability services coordinator to discuss your needs. • Use clear and concise language to explain how your disability impacts your learning and what accommodations you require. 4. Be Proactive in Your Classes • Notify professors of your accommodations early in the semester. • Maintain open communication with your instructors, but remember that you don’t need to disclose your diagnosis—only the accommodations you need. 5. Seek Support When Needed • Utilize campus resources like counseling centers, peer mentoring programs, or academic tutoring. • Join student organizations or support groups for individuals with disabilities to connect with others who share similar experiences. Tips for Building Confidence as a Self-Advocate • Understand Your Strengths and Needs: Self-awareness is key to effective advocacy. Take time to understand your disability, how it impacts you, and what support you require. • Practice Self-Advocacy Skills: Role-play scenarios where you explain your needs or request accommodations. Practicing can help build your confidence. • Be Persistent: If you encounter barriers or resistance, don’t give up. Seek advice from disability services or campus administration if necessary. • Celebrate Your Progress: Every time you successfully advocate for yourself, take pride in your achievement. Advocacy is a skill that grows with time and experience. Empowering Yourself for College Success Understanding your rights and becoming a confident self-advocate puts you in control of your college experience. By securing the accommodations and support you need, you can focus on your education, pursue your passions, and enjoy all that college has to offer. Remember, you’re not alone—there are people and resources ready to support you every step of the way. Take charge of your journey, and don’t be afraid to advocate for the future you deserve.

In any workplace, individuals bring diverse strengths, experiences, and needs. With this diversity comes the inevitable challenge of managing behaviors and interactions that may disrupt workflows or team dynamics. However, not all behaviors are intentional acts of disruption. Some stem from underlying sensory needs, a topic gaining increased attention as organizations strive for inclusivity. So, how can employers and employees differentiate between sensory needs and disruptive behavior and why does understanding this distinction matter? Understanding Sensory Needs Sensory processing refers to how individuals perceive and respond to sensory stimuli, including sound, light, touch, or movement. For some individuals—especially those with conditions like autism, ADHD, or sensory processing disorder—the workplace environment may feel overwhelming. A few examples of sensory challenges that may occur in the workplace include: • Noise Sensitivity : An employee might react to loud or constant sounds, not out of defiance, but because their nervous system is overloaded. • Movement Needs : Some people require frequent movement, such as pacing or fidgeting, to stay focused or regulated. • Lighting Sensitivity : Bright or flickering lights might lead to discomfort, headaches, or distraction. These behaviors are not intentional; they are adaptive responses to environmental stimuli that exceed an individual’s comfort threshold. Disruptive Behavior: A Different Root Cause Disruptive behavior, on the other hand, often arises from external factors like frustration, poor communication, or a lack of engagement. Unlike sensory needs, disruptive actions typically have a clear intent to interrupt or shift the dynamics of the workplace, even if it is subconscious. Examples might include: • Interrupting Colleagues: Cutting others off in meetings without necessity. • Ignoring Policies: Consistently disregarding established norms or expectations. • Negative Attitudes: Complaining, arguing, or refusing to cooperate with team members. Disruptive behaviors often stem from situational factors like stress, dissatisfaction, or poor interpersonal skills, and they require a different approach to resolution. How Employers Can Identify the Difference Distinguishing between sensory needs and disruptive behavior requires careful observation and open communication. Consider the following steps: 1. Look for Patterns: • Sensory-related behaviors often appear in response to specific stimuli (e.g., loud noises or tight spaces). • Disruptive behaviors may appear sporadically and not be tied to external factors. 2. Open a Dialogue: • Approach the individual calmly and inquire about their perspective. Questions like, “I noticed you seem uncomfortable when the office gets noisy. Is there something that might help?” can provide clarity. 3. Seek Professional Input: • Workplace behavior consultants, occupational therapists, or HR specialists trained in inclusivity can help identify if the behavior aligns with a sensory need. 4. Reflect on Context: • Could stress, interpersonal conflict, or burnout be triggering the behavior? If so, consider addressing these factors first. Strategies for a Balanced Workplace Once the cause is identified, appropriate strategies can foster a harmonious environment. If the root cause is Sensory Needs consider the following: • Offer noise-canceling headphones, flexible seating, or adjustable lighting. • Encourage regular breaks to allow for sensory resets. • Provide quiet zones for focused work. If the root cause is Disruptive Behaviors consider the following: • Address conflicts openly with clear communication. • Provide training in emotional intelligence and conflict resolution. • Set clear expectations and boundaries. Building Empathy in the Workplace Understanding the root causes of challenging workplace behaviors is not just a task for HR or management. It’s a shared responsibility that benefits the entire organization. When we approach behavior with curiosity rather than judgment, we create opportunities for growth, inclusion, and collaboration. Distinguishing between sensory needs and disruptive behavior is a nuanced process, but it’s an essential step toward fostering a workplace that accommodates diverse needs while maintaining productivity and harmony. The question isn’t whether to address workplace challenges—it’s how we approach them. By prioritizing empathy, observation, and communication, businesses can transform conflicts into opportunities for greater understanding and inclusion.

Balancing professional duties with caregiving responsibilities can feel like a constant juggling act, with endless to-do lists and competing demands pulling you in multiple directions. For caregivers, the pressure to excel in both areas often leads to feelings of stress, guilt, and exhaustion. However, setting realistic priorities can help create balance and bring a sense of control to your daily life. One of the biggest challenges faced by caregivers who are also professionals is time management. Caregivers often feel like there aren’t enough hours in the day to meet both professional and caregiving responsibilities. Emotional exhaustion and guilt are also significant. Many struggle with the pressure to excel in their careers while also being fully present for their loved ones, leading to burnout. Additionally, there’s the challenge of limited flexibility in workplaces and insufficient support systems at home. Caregivers can approach their employers about their dual responsibilities by being transparent but professional. Share what’s relevant, such as needing flexible hours or remote work, and explain how these adjustments can benefit your productivity. Many employers are open to flexibility if they see that the arrangement won’t compromise performance. It also helps to come prepared with solutions, such as using specific hours for caregiving while maintaining availability during peak work times. Caregivers can set realistic priorities between their work and caregiving responsibilities by understanding what’s most urgent and important in both areas. I recommend using tools like a priority matrix or calendar apps to organize tasks by their level of importance. It’s also essential to communicate with employers and family members about what you can and cannot do. Setting realistic goals and accepting that you can’t do everything perfectly every day helps reduce stress. Delegation is crucial in achieving balance. At work, delegate tasks that others can handle, and focus on your core responsibilities. At home, involve family members or seek external help for caregiving duties. For instance, using services for meal prep, housekeeping, or respite care can significantly lighten the load. It’s about understanding that asking for help isn’t a sign of weakness; it’s a sign of smart planning. Balancing professional duties with caregiving responsibilities while prioritizing self-care requires intentional planning, clear boundaries, and effective use of resources. Here are some practical strategies: 1. Set Priorities • Identify the most critical tasks for your work, caregiving, and self-care. • Use a planner or app to schedule high-priority activities, ensuring each area gets attention. 2. Create a Flexible Routine • Develop a routine that accommodates work and caregiving demands while leaving space for self-care. • Be adaptable and adjust as needed when unexpected events occur. 3. Delegate and Outsource • At work: Delegate tasks to colleagues or employees when possible. • At home: Share caregiving responsibilities with family members or hire professional caregivers if feasible. • Outsource household tasks like cleaning, meal prep, or errands to free up time. 4. Communicate Openly • With your employer: Inform them about your caregiving responsibilities and explore flexible work arrangements like remote work, flex hours, or compressed schedules. • With family: Discuss needs and expectations to ensure everyone shares caregiving responsibilities fairly. 5. Use Technology and Tools • Leverage tools like shared calendars, task management apps, and meal-planning software. • Use caregiving-specific apps for medication reminders or tracking health appointments. 6. Build a Support Network • Connect with friends, family, and community groups for emotional and practical support. • Join caregiving or work-life balance support groups, online or in-person, for advice and encouragement. 7. Set Boundaries • Clearly define work hours and caregiving time to prevent overlap and burnout. • Practice saying no to additional commitments that could overload your schedule. 8. Incorporate Self-Care • Schedule self-care activities like exercise, meditation, or hobbies into your calendar as non-negotiable appointments. • Take short breaks during work or caregiving tasks to recharge. 9. Access Professional Resources • Look into employee assistance programs (EAPs) or caregiver support services. • Seek professional help for stress management, such as therapy or coaching. 10. Practice Mindfulness and Stress Management • Use mindfulness techniques like deep breathing or journaling to stay grounded. • Focus on what you can control and let go of perfectionism. 11. Plan for Emergencies • Have a contingency plan for work and caregiving in case of emergencies, such as backup childcare or alternate caregiving arrangements. 12. Regularly Reassess • Periodically evaluate what’s working and adjust your approach as circumstances change. By combining these strategies and maintaining open communication with all involved parties, you can better balance your responsibilities and maintain your well-being.

Sundowning refers to a group of neuropsychiatric symptoms which commonly develop late afternoon or during the evening and night time ( periods of diminishing daylight). While it is commonly seen in individuals diagnosed with dementia or neurocognitive decline due to #parkinsons or #alzheimers disease, these same symptoms can be seen in children and adults with #autism . When #sundowning becomes apparent, look for patterns, note the things that seem to trigger it, and then do your best to avoid or limit those triggers. We should be our most gentle with individuals who either suffer from Alzheimer's disease or deal with autism the later the day progresses.

Sensory processing disorder (SPD) and (ASD) hold similarities and are often confused with one another. While the two have many similarities, SPD is often a co-morbid symptom (the existence of more than one disease or condition within your body at the same time) of ASD. It is important to note that not all children with sensory processing disorder have autism.